The United Concordia credentialing application process can be a daunting task for many healthcare providers. However, with the right guidance and understanding of the requirements, it can be a relatively smooth and efficient process. In this article, we will break down the United Concordia credentialing application process into manageable steps and provide valuable insights to help simplify the process.
Why is Credentialing Important?
Before we dive into the application process, let's understand why credentialing is crucial for healthcare providers. Credentialing is the process of verifying a healthcare provider's qualifications, education, and experience to ensure they meet the standards of a particular health insurance plan or network. This process helps to ensure that patients receive high-quality care from qualified providers.
Understanding the United Concordia Credentialing Process
United Concordia is a dental insurance company that provides coverage to millions of people across the United States. To become a part of the United Concordia network, healthcare providers must go through the credentialing process. Here's an overview of the steps involved:
- Gather Required Documents: The first step in the credentialing process is to gather all the required documents, including:
- Professional license
- DEA license (if applicable)
- Malpractice insurance
- Education and training certificates
- Board certification (if applicable)
- Complete the Application: Once you have all the required documents, you can complete the United Concordia credentialing application. The application will ask for detailed information about your education, training, and experience.
- Submit the Application: After completing the application, submit it to United Concordia along with the required documents.

Tips to Simplify the Credentialing Process
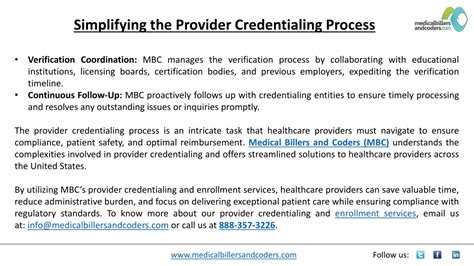
While the credentialing process can be complex, there are several tips to simplify it:
- Start Early: Begin the credentialing process well in advance of your desired start date. This will give you enough time to gather all the required documents and complete the application.
- Use a Credentialing Service: Consider using a credentialing service to help with the application process. These services can help you gather documents, complete the application, and submit it to United Concordia.
- Keep Track of Deadlines: Keep track of deadlines and follow up with United Concordia to ensure that your application is processed in a timely manner.
Common Mistakes to Avoid
While the credentialing process can be complex, there are several common mistakes to avoid:
- Incomplete Applications: Make sure to complete the application fully and accurately. Incomplete applications can delay the credentialing process.
- Missing Documents: Ensure that you have all the required documents before submitting the application.
- Incorrect Information: Double-check the information you provide on the application to ensure it is accurate.

Conclusion
The United Concordia credentialing application process can be complex, but with the right guidance and understanding of the requirements, it can be a relatively smooth and efficient process. By following the tips outlined in this article, you can simplify the credentialing process and ensure that you become a part of the United Concordia network.
Gallery of Credentialing Process






FAQs
What is the United Concordia credentialing process?
+The United Concordia credentialing process is a verification process that ensures healthcare providers meet the standards of the United Concordia network.
What documents are required for the credentialing process?
+The required documents include professional license, DEA license (if applicable), malpractice insurance, education and training certificates, and board certification (if applicable).
How long does the credentialing process take?
+The credentialing process typically takes several weeks to several months, depending on the complexity of the application and the speed of document submission.