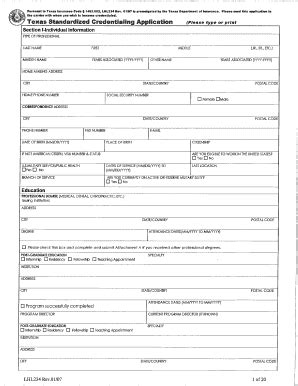
The Texas credentialing application process can be a daunting task for healthcare providers, medical groups, and hospitals. Obtaining the necessary credentials is crucial for reimbursement, licensure, and accreditation purposes. In this article, we will walk you through the step-by-step guide to help you navigate the Texas credentialing application process successfully.

The Importance of Credentialing in Texas
Credentialing is the process of verifying the qualifications, education, and experience of healthcare providers. In Texas, credentialing is mandatory for all healthcare providers who want to participate in the state's Medicaid program or work with private insurance companies. The Texas Medical Board (TMB) and the Texas Department of Insurance (TDI) regulate the credentialing process in the state.
Benefits of Credentialing in Texas
Credentialing offers several benefits to healthcare providers, including:
- Increased reimbursement rates
- Improved patient safety and quality of care
- Enhanced professional reputation
- Compliance with state and federal regulations
- Streamlined administrative processes
Step 1: Gather Required Documents
Before starting the credentialing application process, you need to gather the required documents. These documents include:
- Medical license
- DEA certificate
- Malpractice insurance
- Education and training certificates
- Board certification
- Hospital privileges

Step 2: Choose a Credentialing Organization
There are several credentialing organizations in Texas that can help you with the application process. Some of the most popular organizations include:
- Texas Medical Association (TMA)
- Texas Hospital Association (THA)
- Texas Health Care Association (THCA)
Step 3: Submit the Application
Once you have gathered the required documents and chosen a credentialing organization, you can submit the application. The application process typically involves:
- Completing an online application form
- Uploading required documents
- Paying the application fee

Step 4: Verification and Approval
After submitting the application, the credentialing organization will verify the information and documents provided. This process typically takes several weeks to several months. Once the verification process is complete, the credentialing organization will approve or deny the application.
Tips for a Successful Credentialing Application
To ensure a successful credentialing application, follow these tips:
- Ensure all documents are complete and accurate
- Submit the application well in advance of the deadline
- Follow up with the credentialing organization to ensure the application is being processed
- Be prepared to provide additional information or documentation as required

Conclusion
The Texas credentialing application process can be complex and time-consuming. However, by following the step-by-step guide outlined in this article, you can increase your chances of a successful application. Remember to gather all required documents, choose a reputable credentialing organization, and submit the application well in advance of the deadline. With patience and persistence, you can navigate the Texas credentialing application process and achieve your goals.
Common Challenges in the Credentialing Process
While the credentialing process is designed to ensure that healthcare providers meet certain standards, it can be challenging for providers to navigate. Some common challenges in the credentialing process include:
-
Delays in the Verification Process
The verification process can be time-consuming, and delays can occur if the credentialing organization requires additional information or documentation.
-
Incomplete or Inaccurate Applications
If the application is incomplete or inaccurate, it can be denied or delayed.
-
Lack of Communication
Poor communication between the provider and the credentialing organization can lead to delays or misunderstandings.