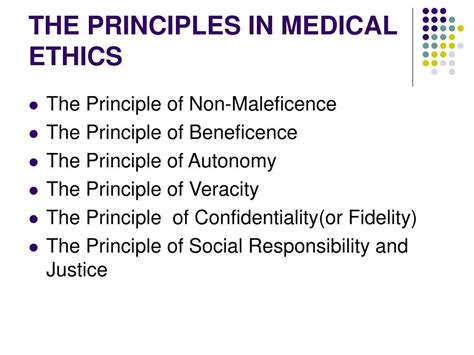
In the field of healthcare, clinical ethics plays a vital role in guiding healthcare professionals to make informed decisions that respect the autonomy, dignity, and rights of patients. The principles of clinical ethics are not merely theoretical constructs, but rather practical guidelines that shape the way healthcare providers interact with patients, families, and communities. In this article, we will explore the 5 key principles of clinical ethics in practice and examine how they influence the delivery of high-quality patient care.
Respect for Autonomy

Respect for autonomy is a fundamental principle in clinical ethics, emphasizing the patient's right to make informed decisions about their care. Healthcare providers must respect patients' autonomy by providing them with accurate and unbiased information, ensuring they understand their diagnosis, treatment options, and potential outcomes. This principle acknowledges that patients have the capacity to make decisions about their own lives and bodies.
In practice, respect for autonomy is demonstrated through:
- Informed consent: Patients must be fully informed about their treatment options and provide explicit consent before any procedure or intervention.
- Patient-centered care: Healthcare providers prioritize patients' values, preferences, and needs when developing care plans.
- Shared decision-making: Patients are encouraged to participate in decision-making processes, ensuring their autonomy is respected and valued.
Non-Maleficence (Do No Harm)

The principle of non-maleficence, or "do no harm," requires healthcare providers to avoid causing harm to patients. This principle is rooted in the Hippocratic Oath and is a cornerstone of clinical ethics. Healthcare providers must carefully balance the benefits and risks of treatment options, ensuring that patients are not subjected to unnecessary harm.
In practice, non-maleficence is demonstrated through:
- Risk-benefit analysis: Healthcare providers weigh the potential benefits of treatment against the potential risks and harms.
- Evidence-based practice: Healthcare providers rely on the best available evidence to inform treatment decisions, minimizing the risk of harm.
- Patient safety initiatives: Healthcare organizations implement policies and procedures to minimize errors and adverse events.
Beneficence (Do Good)

The principle of beneficence, or "do good," requires healthcare providers to act in the best interests of patients, promoting their well-being and quality of life. This principle is closely tied to the concept of patient-centered care, where healthcare providers prioritize patients' needs and values.
In practice, beneficence is demonstrated through:
- Patient-centered care: Healthcare providers prioritize patients' values, preferences, and needs when developing care plans.
- Quality improvement initiatives: Healthcare organizations implement policies and procedures to improve patient outcomes and quality of care.
- Supportive care: Healthcare providers offer emotional, social, and spiritual support to patients and families.
Justice

The principle of justice requires healthcare providers to distribute healthcare resources fairly and equitably, ensuring that patients have access to necessary care regardless of their background, socioeconomic status, or other factors. This principle is closely tied to the concept of social justice, where healthcare providers recognize the broader social determinants of health.
In practice, justice is demonstrated through:
- Access to care: Healthcare providers ensure that patients have access to necessary care, regardless of their background or socioeconomic status.
- Resource allocation: Healthcare organizations allocate resources in a fair and equitable manner, prioritizing patients' needs and values.
- Advocacy: Healthcare providers advocate for patients' rights and interests, promoting social justice and health equity.
Veracity (Truthfulness)

The principle of veracity, or truthfulness, requires healthcare providers to be honest and transparent in their interactions with patients, families, and colleagues. This principle is essential for building trust and promoting informed decision-making.
In practice, veracity is demonstrated through:
- Honest communication: Healthcare providers communicate accurately and transparently with patients, families, and colleagues.
- Disclosure of errors: Healthcare providers disclose errors and adverse events to patients and families, promoting accountability and transparency.
- Informed consent: Patients are fully informed about their treatment options, potential risks, and benefits, ensuring they can make informed decisions.






In conclusion, the 5 key principles of clinical ethics in practice – respect for autonomy, non-maleficence, beneficence, justice, and veracity – provide a foundation for healthcare providers to deliver high-quality patient care that is respectful, compassionate, and equitable. By understanding and applying these principles, healthcare professionals can promote patient-centered care, improve health outcomes, and foster trust and confidence in the healthcare system.
What is the role of clinical ethics in healthcare?
+Clinical ethics plays a vital role in guiding healthcare professionals to make informed decisions that respect the autonomy, dignity, and rights of patients.
What are the 5 key principles of clinical ethics?
+The 5 key principles of clinical ethics are respect for autonomy, non-maleficence, beneficence, justice, and veracity.
How can healthcare providers apply the principle of respect for autonomy?
+Healthcare providers can apply the principle of respect for autonomy by providing patients with accurate and unbiased information, ensuring they understand their diagnosis, treatment options, and potential outcomes.